If you’re a senior struggling with sciatica, gentle movement and targeted exercises can help relieve pain and improve mobility. Sciatica occurs when the sciatic nerve—running from your lower back down through the hips and legs—is irritated or compressed. It’s common in older adults due to spinal wear, posture changes, and decreased flexibility.

Understanding how to move safely is vital. Regular, low-impact stretching and strengthening exercises can ease nerve pressure, enhance posture, and help you stay active—without aggravating symptoms. This guide outlines 10 gentle, senior-friendly exercises for safe, effective relief at home.
Why Sciatica Exercises Matter for Seniors
With age, spinal discs lose cushioning and flexibility, increasing the risk of nerve compression. Targeted exercises can:
- Reduce stiffness and improve range of motion.
- Strengthen the core and glutes to stabilize the spine.
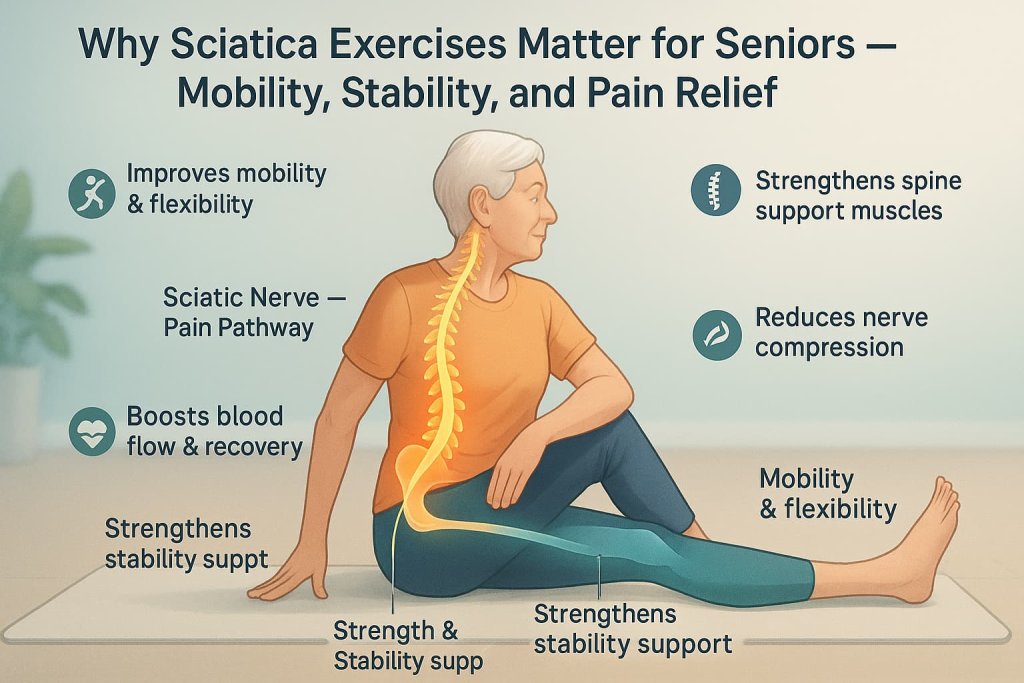
- Increase blood flow for faster recovery.
- Support balance and daily mobility.
Research published in Frontiers in Physiology (2023) and BMC Musculoskeletal Disorders (2024) confirms that gentle stretching and strengthening programs improve function and reduce pain in older adults with low back or sciatic symptoms.
Warm-Up (Always Begin Here)
5–10 minutes of gentle moves boosts circulation and prevents stiffness:
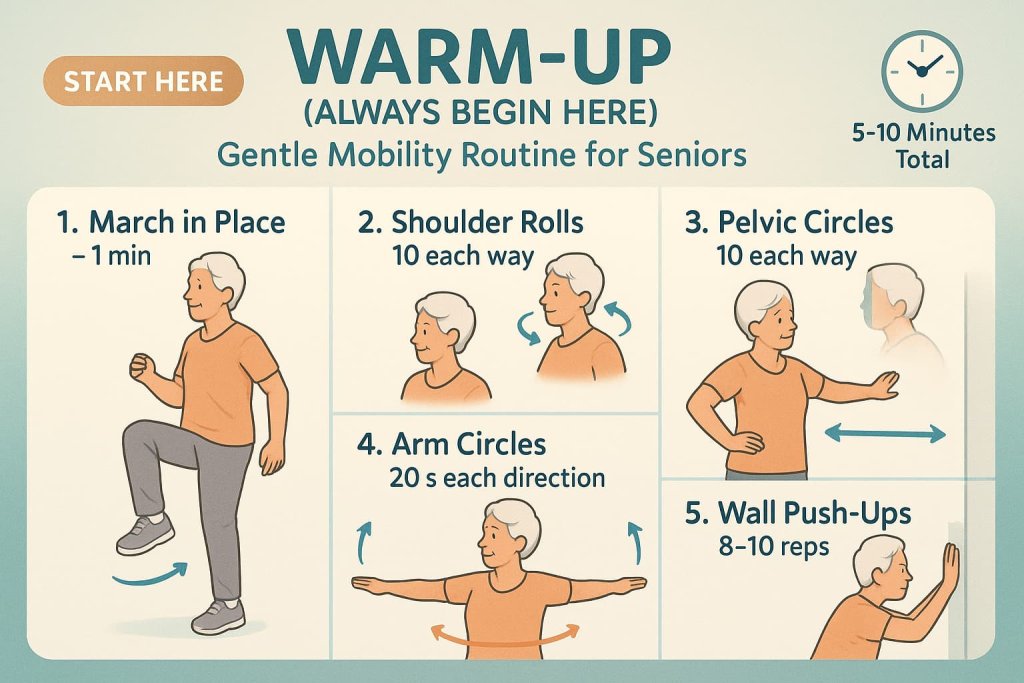
- March in place – 1 min
- Shoulder rolls – 10 each way
- Pelvic circles – 10 each way
- Arm circles – 20 s each direction
- Wall push-ups – 8–10 reps
The 10 Best Sciatica Exercises for Seniors
These gentle, low-impact exercises are designed to relieve sciatic nerve pain, improve flexibility, and strengthen key support muscles without strain.
Each move is safe for seniors, easy to modify, and helps restore comfort and confidence in daily movement.
1. Pelvic Tilt
Why it works:
The pelvic tilt strengthens the deep core muscles (especially the transverse abdominis and pelvic floor) that stabilize your lower spine. It helps reduce the excessive lumbar curve that often compresses the sciatic nerve. This movement retrains your pelvis to maintain a neutral position and alleviates tension from prolonged sitting or poor posture — both common sciatica triggers in seniors.
Muscles worked:
- Transverse abdominis (deep core)
- Rectus abdominis (front abs)
- Gluteus medius and minimus (light engagement)
- Lumbar stabilizers and pelvic floor muscles
How to do it:
- Lie flat on your back with your knees bent and feet hip-width apart.
- Keep your arms relaxed by your sides, palms facing down.
- Inhale gently to prepare.
- As you exhale, draw your belly button toward your spine and flatten your lower back against the floor.
- Tilt your pelvis backward slightly so your tailbone moves down toward the floor.
- Hold for 5–10 seconds, maintaining steady breathing.
- Relax and return to the starting position.
- Repeat 10–12 slow, controlled reps.
Trainer Tip:
Focus on slow, controlled muscle engagement rather than large movement. Visualize your pelvis as a bowl of water — during the tilt, tip it just enough so the “water” would pour slightly toward your belly button.
2. Glute Bridge
Why it works:
This exercise strengthens the glutes, hamstrings, and lower back, which together support your spine and reduce sciatic nerve strain. Weak glutes are a major contributor to lower back pain because they shift workload to the lumbar spine. The glute bridge restores balance and improves hip stability, helping you walk and stand taller.
Muscles worked:
- Gluteus maximus (primary mover)
- Hamstrings
- Erector spinae (spinal stabilizers)
- Core (transverse abdominis, obliques)
How to do it:
- Lie on your back with knees bent and feet flat on the floor, hip-width apart.
- Engage your abdominal muscles to protect your spine.
- Press your heels into the floor and squeeze your glutes as you lift your hips slowly.
- Lift only until your body forms a straight line from shoulders to knees.
- Hold for 3–5 seconds, then lower your hips down in a controlled manner.
- Perform 8–10 reps, 1–2 sets.
Trainer Tip:
If you feel the movement in your lower back instead of your glutes, reduce the lift height and consciously squeeze your glutes at the top. For additional support, place a small pillow under your lower back or hips.
3. Seated Hamstring Stretch
Why it works:
Tight hamstrings can tilt your pelvis backward and flatten the lumbar spine, increasing nerve pressure and sciatic discomfort. This gentle seated version is ideal for seniors as it improves flexibility and circulation without straining the back.
Muscles worked:
- Hamstrings (biceps femoris, semitendinosus, semimembranosus)
- Gastrocnemius and soleus (calf muscles)
- Gluteal base (mild)
How to do it:
- Sit tall at the edge of a sturdy chair.
- Extend one leg forward with the heel on the floor and toes pointing up.
- Keep your back straight and shoulders relaxed.
- Gently hinge forward from the hips — avoid rounding your spine.
- Stop when you feel a comfortable stretch along the back of your thigh.
- Hold for 20–30 seconds, breathing evenly.
- Return to upright posture and switch legs.
- Repeat 2–3 times per side.
Trainer Tip:
For extra support, loop a towel or yoga strap around the extended foot. Avoid bouncing; this stretch should feel like a steady lengthening, not a pull.
4. Figure-4 (Piriformis) Stretch
Why it works:
The piriformis muscle, located deep in the buttock, often compresses the sciatic nerve when tight — a condition known as piriformis syndrome. This stretch releases that tension, improving nerve gliding and hip mobility.
Muscles worked:
- Piriformis
- Gluteus medius and minimus
- Tensor fasciae latae (TFL)
- External hip rotators
How to do it:
- Sit upright on a chair with your feet flat on the ground.
- Cross your right ankle over your left knee, forming a “figure-4.”
- Keep your spine tall and hinge slightly forward from the hips until you feel a gentle stretch in your right hip and buttock.
- Hold for 20–30 seconds.
- Slowly return to start and switch sides.
- Repeat 2–3 times per side.
Trainer Tip:
Don’t force the leg into position — use gravity and gentle movement. If your hips are tight, place a small cushion under your elevated leg for comfort.
5. Knee-to-Chest Stretch
Why it works:
This stretch gently opens the lower spine, easing compression on the nerve roots that form the sciatic nerve. It also relaxes the glutes and lower back muscles, reducing tension after prolonged sitting.
Muscles worked:
- Gluteus maximus
- Lumbar paraspinals
- Hip flexors (on opposite leg)
How to do it:
- Lie flat on your back with knees bent.
- Bring one knee toward your chest, holding behind your thigh or below the knee (not on the kneecap).
- Keep the other foot flat on the floor.
- Hold for 15–30 seconds, breathing deeply.
- Lower slowly and switch legs.
- Repeat 2–3 times per side.
Trainer Tip:
If lying flat causes discomfort, perform this stretch with one foot resting on a low step or bed. Keep shoulders relaxed and avoid lifting your head.
6. Seated Spinal Twist
Why it works:
Improves rotational flexibility of the spine, relieves stiffness in the lower back, and helps balance muscular tension between both sides of the body. Controlled twisting increases mobility without loading the joints — ideal for seniors with limited flexibility.
Muscles worked:
- Obliques
- Erector spinae (multifidus and longissimus)
- Hip rotators
How to do it:
- Sit tall in a firm chair with feet flat on the ground.
- Place your right hand on the outside of your left knee and your left hand on the chair’s backrest.
- Inhale deeply to lengthen your spine.
- Exhale and gently twist your torso toward the left.
- Hold 15–20 seconds, feeling a gentle stretch in your mid and lower back.
- Return to center and switch sides.
- Perform 2–3 rounds per side.
Trainer Tip:
Think “lift before twist” — elongate your spine before turning. Avoid forcing the rotation; the movement should be smooth and comfortable.
7. Seated Back Bend (Extension)
Why it works:
This gentle back extension strengthens spinal extensors and helps maintain natural lumbar curvature, which is often lost in seniors due to forward stooping. Extension also creates more space in the spinal canal, which can ease mild nerve compression.
Muscles worked:
- Erector spinae
- Gluteus maximus
- Hip flexors (stretched)
How to do it:
- Sit tall in a sturdy chair, feet planted.
- Place your hands on your lower back or the sides of your chair for support.
- Slowly lift your chest and arch your back slightly, gazing upward.
- Hold 5–10 seconds, then return to neutral.
- Repeat 5–8 times.
Trainer Tip:
Keep the motion small and pain-free. You should feel gentle stretching in the abdomen and front hips, not pinching in your lower back.
8. Bird Dog (Wall-Supported)
Why it works:
This modified Bird Dog builds spinal stability without requiring kneeling on the floor—perfect for seniors with balance issues or knee discomfort. It strengthens opposing muscle chains and improves coordination, posture, and balance.
Muscles worked:
- Core stabilizers (transverse abdominis, multifidus)
- Gluteus maximus and medius
- Hamstrings
- Posterior shoulders and upper back
How to do it:
- Stand facing a wall, hands flat on it at shoulder height.
- Step your feet back until your body forms a straight line from head to heels.
- Tighten your core and lift your right arm forward while extending your left leg back.
- Keep your hips level and spine neutral.
- Hold 2–3 seconds, then return slowly.
- Repeat 10 reps per side.
Trainer Tip:
Imagine balancing a cup of water on your lower back — no spills! Keep movements slow and deliberate.
9. Calf Stretch (Wall)
Why it works:
Tight calf muscles can alter walking mechanics and increase stress up the kinetic chain — especially in seniors who walk less frequently. Stretching them improves ankle mobility, posture, and balance, reducing compensatory strain on the lower back.
Muscles worked:
- Gastrocnemius (upper calf)
- Soleus (deep calf)
- Achilles tendon
How to do it:
- Stand facing a wall, hands on the wall at shoulder level.
- Step one leg back, keeping heel on the ground and toes facing forward.
- Bend your front knee slightly while keeping the back leg straight.
- Lean forward gently until you feel a stretch in the back calf.
- Hold 20–30 seconds, then switch sides.
- Repeat 2–3 rounds per leg.
Trainer Tip:
For a deeper soleus stretch, slightly bend your back knee while keeping the heel down. Maintain upright posture — avoid hunching forward.
10. Gentle Walking
Why it works:
Walking promotes blood circulation, joint mobility, and nerve health without the impact of running or jumping. It helps reduce stiffness, strengthens the glutes and legs, and supports a healthy spine. Even short walks can reduce pain intensity in seniors with sciatica when done consistently.
Muscles worked:
- Gluteus maximus and medius
- Hamstrings and quadriceps
- Core stabilizers
- Calves and ankles
How to do it:
- Start with a 5–10-minute walk on a flat, even surface (indoors or outdoors).
- Keep an upright posture, relaxed shoulders, and natural arm swing.
- Gradually increase duration by 1–2 minutes each week as tolerated.
- Aim for 15–20 minutes per day, 3–5 days per week.
Trainer Tip:
Wear supportive walking shoes and maintain a moderate pace — brisk enough to increase your breathing slightly but comfortable enough to hold a conversation. If symptoms flare, take short, frequent walks instead of one long session.
How to Use This Routine
- Frequency: 2–3 times weekly.
- Sets/Reps: 1 set of 8–12 reps (20–30 s holds).
- Equipment: Chair, wall, supportive shoes.
- Progression: Add reps or time gradually.
- Combine with: Light daily walking and hydration.
Common Mistakes to Avoid
- Stretching too forcefully or bouncing.
- Holding your breath during movements.
- Skipping warm-up.
- Sitting too long between exercises.
- Ignoring new symptoms like tingling or weakness.
Progression Plan
| Phase | Frequency | Sets/Reps | Notes |
|---|---|---|---|
| Weeks 1–2 | 2–3 times/week | 1 set each | Focus on comfort & control |
| Weeks 3–4 | 3 times/week | 2 sets each | Slightly increase hold time |
| Week 5+ | 3–4 times/week | 2 sets + 10-15 min walk | Maintain consistency |
Safety & Precautions
Before starting, review these safety rules:
- Consult your doctor or physical therapist before beginning any new routine.
- Stop immediately if pain radiates, tingles, or worsens down the leg.
- Warm up gently for 5–10 minutes (marching in place or light walking).
- Avoid jerky or twisting movements.
- Perform exercises on a firm, non-slippery surface.
- Breathe steadily—never hold your breath.
- Focus on quality and comfort over quantity.
FAQs
1. Can seniors safely exercise with sciatica?
Yes. When exercises are gentle, slow, and approved by a professional, they can safely reduce symptoms and improve mobility.
2. Should I rest during a flare-up?
Avoid complete bed rest. Light movement helps recovery.
3. What if my leg tingles during exercise?
Stop the movement. Tingling may indicate nerve irritation.
4. How long until I feel results?
Consistent daily practice (2–4 weeks) often brings gradual relief.
5. What should I avoid?
Heavy lifting, twisting, and forward bending with straight legs.
6. Do I need equipment?
Just a chair, wall, and supportive shoes.
7. When should I see a doctor?
If pain worsens, or if you experience weakness, numbness, or bladder/bowel issues.
Conclusion
Sciatica doesn’t have to keep you sidelined. With these 10 gentle, senior-friendly exercises, you can regain flexibility, strengthen supporting muscles, and reduce nerve pain safely at home.
Start small—commit to one routine this week. Over time, you’ll notice improved posture, balance, and daily comfort.
Disclaimer:
This content is for informational purposes only and is not medical advice. Always consult your doctor or physical therapist before starting new exercises.
References
- NICE Guideline NG59 — Low Back Pain and Sciatica in Over 16s (Assessment & Management)
NICE NG59 - ACP Clinical Practice Guideline — Noninvasive Treatments for Low Back Pain (Qaseem et al., 2017)
Annals of Internal Medicine (ACP Guideline) - Sciatica — Clinical Review (Ropper & Zafonte, 2015)
New England Journal of Medicine - Exercise Therapy for Chronic Low Back Pain — Systematic Review & Meta-analysis (Cochrane, 2021; Hayden et al.)
Cochrane Library - WHO Guidelines on Physical Activity and Sedentary Behaviour (2020)
World Health Organization
