The best COPD breathing exercises may help you breathe easier by improving airflow, reducing shortness of breath, and increasing your breathing control. These exercises support lung efficiency, help slow your breathing rate, and make daily activities feel more manageable.

Understanding how to use the right breathing techniques is important because COPD affects how air moves in and out of the lungs. These exercises can support better breathing patterns, help reduce air trapping, and improve comfort—especially during physical activity or flare-ups.
Below you’ll find the 6 best COPD breathing exercises, step-by-step instructions, safety guidelines, and tips based on recommendations from major organizations such as the American Lung Association, COPD Foundation, and pulmonary rehabilitation frameworks.
What Are COPD Breathing Exercises?
COPD breathing exercises are controlled breathing techniques designed to support better oxygen flow, reduce breathlessness, and help your lungs work more efficiently. These exercises are often taught in pulmonary rehabilitation programs, and they can be practiced at home as part of daily self-care.
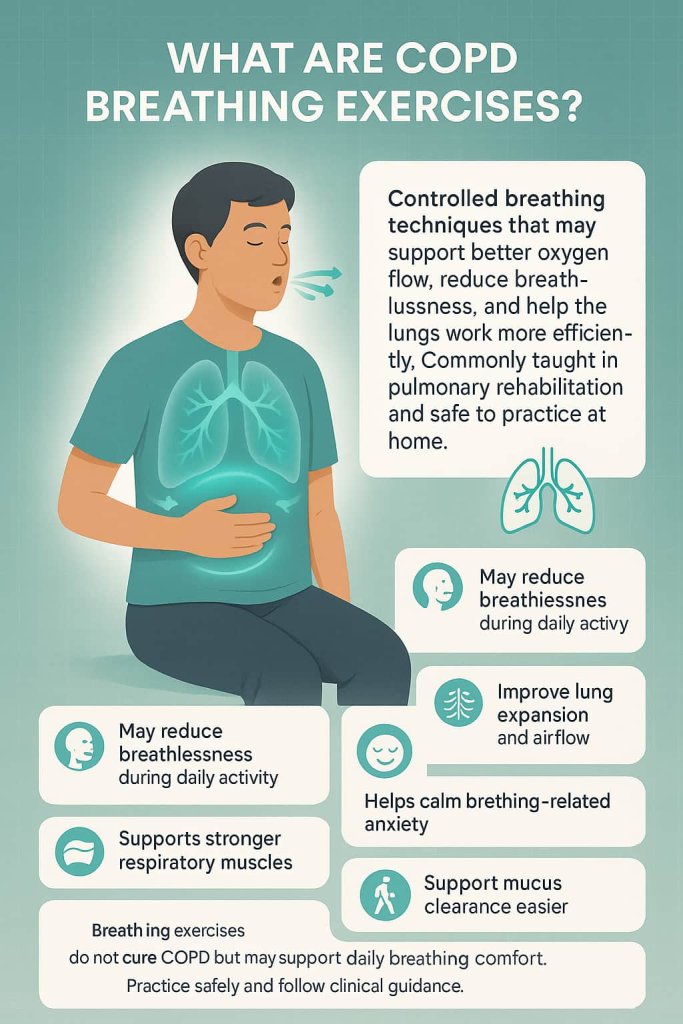
Benefits of COPD Breathing Exercises
Breathing exercises for COPD may help:
- Reduce breathlessness during activity
- Improve lung expansion and airflow
- Strengthen respiratory muscles
- Reduce anxiety caused by shortness of breath
- Improve exercise tolerance
- Support easier mucus clearance
- Improve overall quality of life
While these exercises do not cure COPD, they can support better day-to-day breathing and complement your medical treatment plan.
What to Know Before Starting COPD Breathing Exercises
Before beginning COPD breathing exercises, follow these key safety points to ensure you practice comfortably and safely. These guidelines help reduce the risk of increased breathlessness and support better breathing control.
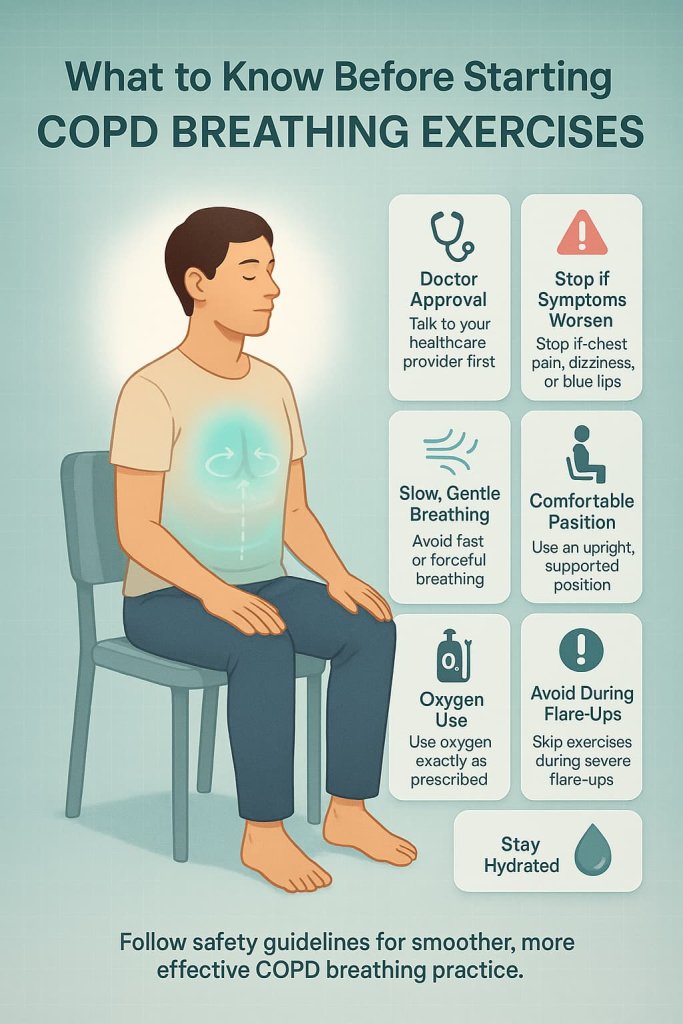
- Talk to your healthcare provider first, especially if you have severe COPD, frequent flare-ups, heart conditions, or use supplemental oxygen.
- Stop immediately if you feel chest pain, dizziness, severe breathlessness, or notice blue lips or fingertips.
- Breathe slowly and gently—avoid forceful or rapid breathing, which can worsen air trapping.
- Use a comfortable position, such as upright sitting, to allow your diaphragm to move freely.
- Keep your shoulders, neck, and jaw relaxed to reduce unnecessary muscle tension.
- Use oxygen exactly as prescribed; never adjust flow rates without medical guidance.
- Avoid practicing during a severe flare-up unless your doctor has instructed otherwise.
- Stay well hydrated to help loosen mucus and support airway clearance techniques.
These simple precautions make breathing exercises safer and more effective for everyday COPD symptom management.
6 Best COPD Breathing Exercises That Help You Breathe Easier Every Day
These six COPD breathing exercises are simple, safe, and designed to help you manage breathlessness more effectively. Each technique supports better airflow, improves breathing control, and can be practiced at home every day.
1. Pursed-Lip Breathing (PLB)
Best for: Reducing breathlessness and preventing air trapping
Why It Works
Pursed-lip breathing slows the rate of exhalation and helps keep the small airways open longer. This may reduce the amount of air trapped in the lungs—one of the main challenges in COPD. By controlling airflow, PLB can ease shortness of breath during rest and activity.
Muscles Worked
- Diaphragm
- Intercostal muscles (muscles between the ribs)
- Accessory breathing muscles (used more efficiently, with less strain)
How to Do It
- Sit or stand tall with relaxed shoulders.
- Inhale gently through your nose for about 2 seconds.
- Purse your lips as if blowing out a candle.
- Exhale slowly for 4–6 seconds, about twice as long as the inhale.
- Repeat for 1–2 minutes, or as needed during breathlessness.
Trainer Tip
Use PLB anytime you feel short of breath—walking, climbing stairs, or after light activity. The longer, slower exhale is the key to reducing air trapping.
2. Diaphragmatic (Belly) Breathing
Best for: Strengthening the diaphragm and reducing the work of breathing
Why It Works
COPD often forces people to rely more on accessory neck and chest muscles. Diaphragmatic breathing teaches the body to use the diaphragm more effectively, which may reduce breathing effort and promote deeper, more efficient inhalation.
Muscles Worked
- Diaphragm (primary target)
- Abdominal muscles (gentle activation during exhale)
- Lower intercostals
How to Do It
- Lie down or sit comfortably with one hand on your belly.
- Inhale through your nose so your belly gently rises under your hand.
- Exhale slowly through pursed lips as your belly falls.
- Keep shoulders relaxed and avoid chest lifting.
- Repeat 5–10 cycles, working toward smooth rhythmical breathing.
Trainer Tip
If your chest rises more than your belly, slow down and place a light book on your abdomen. This helps reinforce proper diaphragmatic movement.
3. Huff Coughing (Airway Clearance Technique)
Best for: Clearing mucus without excessive strain
Why It Works
COPD can cause mucus buildup that makes breathing more difficult. Huff coughing creates strong airflow through the airways while minimizing throat irritation and energy expenditure. It is a gentler alternative to forceful coughing.
Muscles Worked
- Abdominal muscles
- Diaphragm
- Expiratory respiratory muscles
How to Do It
- Take a medium-sized breath in.
- Hold it for 1–2 seconds.
- Exhale forcefully through an open mouth while saying “ha, ha, ha.”
- Think of fogging up a mirror—steady, controlled, not harsh.
- Repeat 2–3 times as needed.
Trainer Tip
Use huff coughing after PLB or deep breathing to help move mucus upward. Always stay hydrated to make mucus easier to clear.
4. Paced Breathing During Activity
Best for: Reducing breathlessness during walking, climbing stairs, or lifting
Why It Works
Coordinating breath with movement reduces strain on the lungs. Paced breathing helps maintain steady airflow, prevents rapid breathing spikes, and makes physical tasks feel more manageable.
Muscles Worked
- Diaphragm
- Intercostals
- Core muscles (stabilizing during movement)
How to Do It
- Inhale gently before starting the movement.
- Exhale through pursed lips during the effort phase.
Examples:
- Climbing stairs: inhale → step → exhale → next step
- Walking: inhale for 1–2 steps, exhale for 2–4 steps
Trainer Tip
The exhale should always match the effort. Use PLB as your exhale technique to stay in control throughout activity.
5. Deep Breathing (Segmental Expansion)
Best for: Expanding lung areas that tend to collapse or tighten
Why It Works
Deep, controlled inhalation helps improve airflow to underused lung segments. This may reduce shallow breathing patterns and enhance chest expansion, making each breath more efficient.
Muscles Worked
- Diaphragm
- Intercostals
- Upper and lower rib cage stabilizers
How to Do It
- Sit upright with relaxed shoulders.
- Place your hands on your ribcage or sides.
- Inhale slowly through your nose, feeling your ribs push outward.
- Hold for 1–2 seconds.
- Exhale slowly through pursed lips.
- Repeat 6–8 breaths.
Trainer Tip
Gently press your hands into your ribs as you inhale—this gives your lungs something to expand against and improves awareness of rib movement.
6. Forward-Leaning / Tripod Position + Breathing
Best for: Quickly reducing shortness of breath
Why It Works
The forward-leaning posture stabilizes the upper body and allows the diaphragm to contract more effectively. It also relaxes accessory neck and shoulder muscles, making each breath easier and more efficient—especially during sudden breathlessness.
Muscles Worked
- Diaphragm (better positioning for activation)
- Intercostals
- Accessory muscles (reduced strain)
How to Do It
- Sit or stand with a gentle forward lean.
- Rest your hands on your thighs, knees, or a table.
- Relax your neck and shoulders completely.
- Use slow, controlled pursed-lip breathing.
- Continue until breathing eases.
Trainer Tip
This position is especially effective during flare-ups or after exertion. Add PLB for even faster relief.
How Often Should You Do COPD Breathing Exercises?
Most experts recommend:
- Daily practice for 5–10 minutes
- Using PLB and paced breathing as needed during symptoms
- Using huff coughing whenever mucus builds up
- Adding diaphragmatic breathing 3–4 times per day for best results
In pulmonary rehabilitation, breathing exercises are practiced regularly along with physical activity.
Safety Guidelines for COPD Breathing Exercises
- Always check with your doctor or pulmonary rehab specialist before starting new breathing routines.
- Stop if you feel:
- Chest pain
- Dizziness or faintness
- Severe or worsening breathlessness
- Blue lips or fingertips
- Avoid very fast or forceful breathing.
- Use a quiet, relaxed environment to prevent tension.
- If you use supplemental oxygen, follow your prescribed settings.
Frequently Asked Questions (FAQ)
1. Can breathing exercises improve COPD?
Breathing exercises do not cure COPD, but they may help improve airflow, reduce shortness of breath, and support better daily breathing control.
2. How long does it take to notice results?
Many people feel more comfortable breathing after just a few sessions, but consistent daily practice offers better long-term benefits.
3. Should I use oxygen while doing these exercises?
Use oxygen exactly as prescribed. If unsure, ask your healthcare provider or pulmonary rehab therapist.
4. Are these exercises safe during a COPD flare-up?
Some techniques—like PLB and tripod breathing—can help during flare-ups, but always follow medical guidance if symptoms worsen.
5. Can breathing exercises replace medications?
No. They support breathing comfort but do not replace inhalers, treatments, or medical care.
6. Do these exercises help with anxiety caused by shortness of breath?
Yes. Slow, controlled breathing may help calm anxiety that often accompanies breathing difficulty.
7. Should seniors with COPD do these exercises?
Yes—these techniques are widely used in pulmonary rehabilitation programs for older adults.
Conclusion
COPD breathing exercises are simple, accessible tools that may help you breathe easier, reduce shortness of breath, and support better daily function. Practicing these six techniques regularly can make activities like walking, climbing stairs, and talking more comfortable.
If you want the best results, combine these exercises with pulmonary rehabilitation, your prescribed treatments, and ongoing communication with your healthcare provider.
This content is for informational purposes only and not medical advice.
References
- GOLD 2025 – Global Strategy for COPD
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of COPD: 2025 Report.
https://goldcopd.org/2025-gold-report/ - Pulmonary Rehabilitation Overview (Exercise + Breathing)
Arnold MT, Soicher JE, Luckett T, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease: A narrative review of current evidence. ERJ Open Res. 2020.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7515680/ - Breathing Exercises in COPD – Overview of Systematic Reviews
Li Y, Wang Y, Chen L, et al. Breathing exercises in the treatment of COPD: an overview of systematic reviews. COPD. 2022.
https://www.dovepress.com/breathing-exercises-in-the-treatment-of-copd-an-overview-of-systematic-peer-reviewed-fulltext-article-COPD - Breathing Exercises Meta-Analysis (Dyspnea, Function, QoL)
Ubolnuar N, Tantisira MH, Harnmontree P, et al. Effects of breathing exercises in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clin Rehabil. 2019.
https://pubmed.ncbi.nlm.nih.gov/31499605/ - Pursed-Lip Breathing – Clinical Overview
Nguyen JD, et al. Pursed-lip breathing. StatPearls [Internet]. 2023.
https://www.ncbi.nlm.nih.gov/books/NBK545289/ - Pursed-Lip Breathing – Technique & Benefits (Patient-Friendly)
Cleveland Clinic. Pursed lip breathing: technique, purpose & benefits.
https://my.clevelandclinic.org/health/treatments/9443-pursed-lip-breathing - Diaphragmatic Breathing – COPD Trial
Fernandes M, et al. Efficacy of diaphragmatic breathing in patients with chronic obstructive pulmonary disease. Respir Med. 2011.
https://pubmed.ncbi.nlm.nih.gov/22094449/ - Huff Coughing – How-To & Purpose
Cleveland Clinic. Huff cough: huffing, maneuver, purpose & how to.
https://my.clevelandclinic.org/health/treatments/8697-huff-cough
