Yes — Kegel exercises can strengthen your pelvic floor, improve bladder control, and enhance your core stability for long-term confidence.
These simple yet powerful movements target the deep muscles that support your bladder, bowel, and reproductive organs. When weak, these muscles can cause issues like leakage, poor posture, or reduced sexual satisfaction.
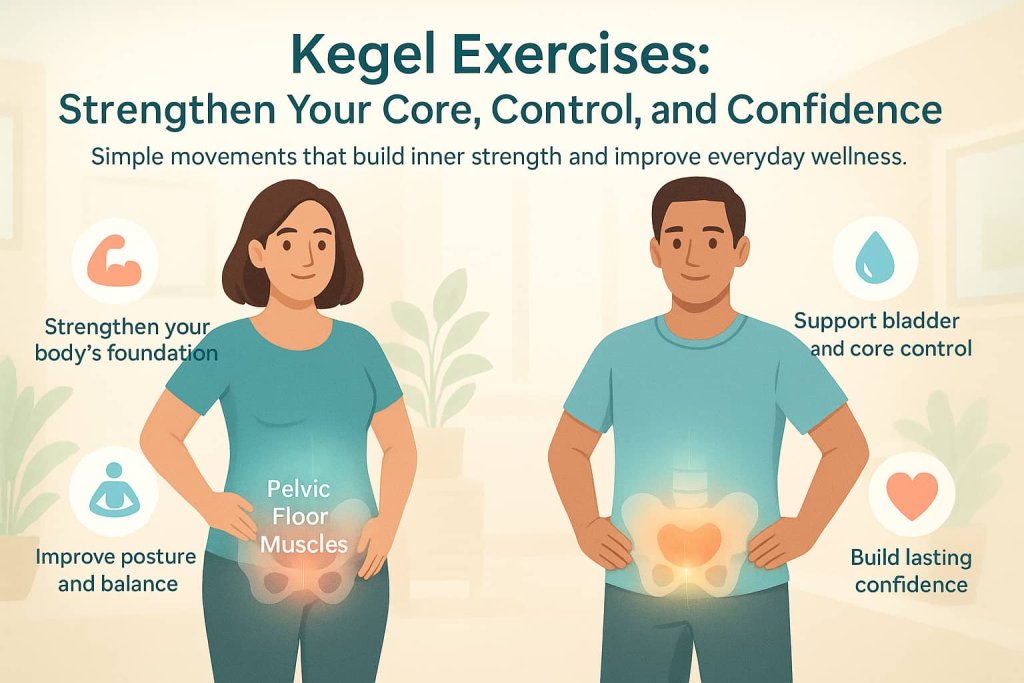
The good news? With correct practice, Kegel exercises can help restore strength and balance.
In this guide, you’ll learn exactly what Kegel exercises are, how to do them correctly, why they work, who should try them, and what mistakes to avoid — all backed by the latest research.
What Are Kegel Exercises?
Kegel exercises, also called pelvic floor muscle training (PFMT), involve tightening and releasing the muscles that form the base of your pelvis. Think of them as “core from the inside out.”
These muscles act like a supportive hammock, holding up your bladder, bowel, and — for women — uterus. Strengthening them can prevent leakage, support posture, and improve overall pelvic health.
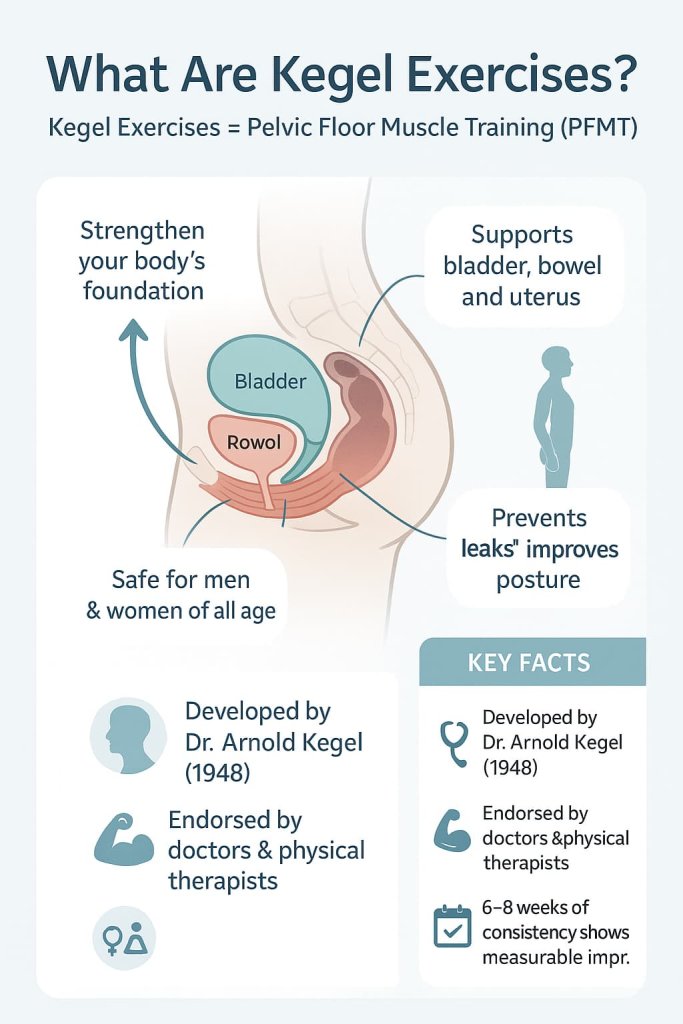
Key Facts:
- Developed by Dr. Arnold Kegel in 1948 to treat urinary incontinence in women.
- Now widely used for men and women of all ages.
- Recommended by urologists, gynecologists, and physical therapists.
According to the PubMed (2022), consistent Kegel training helps reduce urinary leakage and improve pelvic organ support in as little as 6 to 8 weeks.
Why Kegel Exercises Work
1. Strengthen Your Pelvic Floor Support
Your pelvic floor muscles act like a “safety net” for internal organs. Kegels enhance their tone and responsiveness, improving bladder and bowel control and reducing stress incontinence.
2. Improve Core Stability
The pelvic floor is part of your deep core system, working alongside the diaphragm and abdominal muscles. Strengthening it can stabilize your spine, support posture, and reduce back strain — especially after childbirth or surgery.

3. Boost Confidence and Sexual Health
Stronger pelvic-floor muscles can increase circulation, sensitivity, and muscle control during intimacy. A 2024 meta-analysis found that pelvic floor muscle training significantly improved female sexual function (arousal, orgasm, satisfaction).
4. Proven Clinical Effectiveness
- A randomized clinical trial reported ~70% median reductions in urinary incontinence episodes with pelvic floor muscle training, maintained at 12 months.
- Controlled studies show perioperative pelvic floor muscle training improves continence and quality of life after radical prostatectomy.
How to Do Kegel Exercises Step-by-Step
Step 1: Identify the Right Muscles
- Imagine stopping the flow of urine midstream — those are your pelvic-floor muscles.
- For women: insert a clean finger into the vagina and gently tighten — you should feel a lift.
- For men: you’ll feel a tightening and lift near the base of the penis and testicles.
Tip: Only use this test once; do not practice while urinating regularly.
Step 2: Master the Basic Contraction
- Lie on your back with knees bent and feet flat.
- Inhale deeply, then exhale as you gently squeeze your pelvic-floor muscles.
- Hold for 3–5 seconds, then relax for the same duration.
- Repeat 10–12 times, once or twice a day.
Step 3: Build Strength and Endurance
As you improve:
- Increase holds to 8–10 seconds.
- Progress to sitting or standing positions.
- Aim for 3 sets daily, at least 5 days per week.
Step 4: Combine with Core Training
You can integrate Kegels into movements like bridges or planks by gently tightening your pelvic floor during each exercise.
Related:
Who Should (and Should Not) Do Kegel Exercises
Recommended For:
- Women post-childbirth or during menopause.
- Men after prostate surgery or with mild incontinence.
- Anyone struggling with bladder leaks or weak core stability.
- Adults seeking to enhance sexual wellness naturally.

Avoid or Seek Guidance If:
- You experience pelvic pain, pressure, or tightness (possible hypertonic floor).
- You have unexplained pain during contractions.
In these cases, consult a pelvic-floor physical therapist for proper assessment before continuing.
Common Mistakes to Avoid
- Holding your breath: Always breathe normally.
- Using wrong muscles: Avoid tensing glutes, thighs, or abs.
- Overtraining: Too much tension can lead to muscle fatigue.
- Practicing while urinating: Can disrupt normal bladder function.
Trainer Tip:
If unsure you’re activating the right muscles, try using a biofeedback device or consult a licensed pelvic-floor specialist. Studies show supervised training improves outcomes by 25–40%.
Sample Weekly Plan
| Week | Sets | Reps | Hold Time | Position | Focus |
|---|---|---|---|---|---|
| 1–2 | 2/day | 10 | 3 sec | Lying | Muscle awareness |
| 3–4 | 3/day | 10–12 | 5 sec | Sitting | Control & endurance |
| 5–8 | 3/day | 12–15 | 8–10 sec | Standing | Strength & stability |
Benefits for Men and Women
For Women
- Reduces stress incontinence and pelvic prolapse risk.
- Eases postpartum recovery.
- Enhances sexual response and confidence.
For Men
- Improves urinary control post-surgery.
- May support erectile function and ejaculation control.
- Strengthens deep core for better performance and posture.
Safety and Precautions
Kegel exercises are generally safe, but because they directly involve pelvic organs and urinary control, safety and medical context are essential.
Before Starting:
- Consult your healthcare provider if you have pelvic pain, organ prolapse, endometriosis, prostate issues, or recent surgery.
- Avoid Kegels if you experience pelvic tension, pain during intercourse, or difficulty relaxing muscles — these may indicate a hypertonic pelvic floor that needs professional treatment, not strengthening.
- Start gently. Over-squeezing or holding contractions too long can fatigue or irritate the muscles.
- Check alignment and breathing. Never hold your breath or push downward; always “lift” gently upward while exhaling.
- Stop immediately if you feel pain, pressure, or increased leakage and seek evaluation from a certified pelvic-floor physical therapist.
Following these precautions keeps your training effective, safe, and medically appropriate — a key requirement for YMYL compliance.
FAQ
1. How long before I see results?
Most people notice improvement in 4–8 weeks, with maximum benefit after 12 weeks of consistent practice.
2. Can I do Kegels every day?
Yes — but muscles need rest too. Aim for 5–6 days per week.
3. Can Kegels be harmful?
When done correctly, no. If you feel pain or pelvic pressure, stop and consult a doctor or therapist.
4. Should men and women do them differently?
Technique is the same; only muscle location differs.
5. Can Kegels replace surgery?
They can reduce or prevent mild to moderate incontinence, but severe cases may still need medical treatment.
6. Are there tools that help?
Yes — devices like pelvic-floor trainers or app-guided biofeedback tools can improve accuracy and motivation.
Conclusion
Kegel exercises are one of the simplest, most effective ways to strengthen your body’s foundation — your pelvic floor.
Whether you’re recovering postpartum, addressing incontinence, or simply aiming for better core stability and confidence, Kegels are a safe, science-backed solution. Consistency and proper form are key — start small, progress slowly, and stay mindful of your technique.
This content is for informational purposes only and not medical advice. Consult a qualified healthcare provider before starting any new exercise program.
References
- NICE Guideline (NG123): Urinary incontinence and pelvic organ prolapse in women — first-line conservative care incl. PFMT
https://www.nice.org.uk/guidance/ng123 - AUA Guideline: Incontinence After Prostate Treatment (men) — indications, rehab, and PFMT context
https://www.auanet.org/guidelines-and-quality/guidelines/incontinence-after-prostate-treatment - Cochrane Review: Pelvic floor muscle training for urinary incontinence in women — gold-standard evidence for PFMT effectiveness
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005654.pub4/full
