Heel pain when walking is most often caused by plantar fasciitis—a condition involving strain or degeneration of the tissue under your foot—and it can usually be relieved with rest, stretching, and supportive footwear.
However, there are several other possible causes, and understanding them is the first step to lasting relief.

Why Heel Pain Shouldn’t Be Ignored
Your heel is the largest bone in your foot and takes the brunt of every step. With each stride, it absorbs forces of 1.5 to 3 times your body weight. Even minor injuries or repetitive stress can quickly lead to inflammation, tissue damage, and long-term foot problems. Ignoring heel pain may cause your body to shift weight abnormally, which can lead to knee, hip, or back pain.
Key takeaway: Early diagnosis and treatment not only help you recover faster but also prevent chronic pain and mobility loss.
Main Causes of Heel Pain When Walking
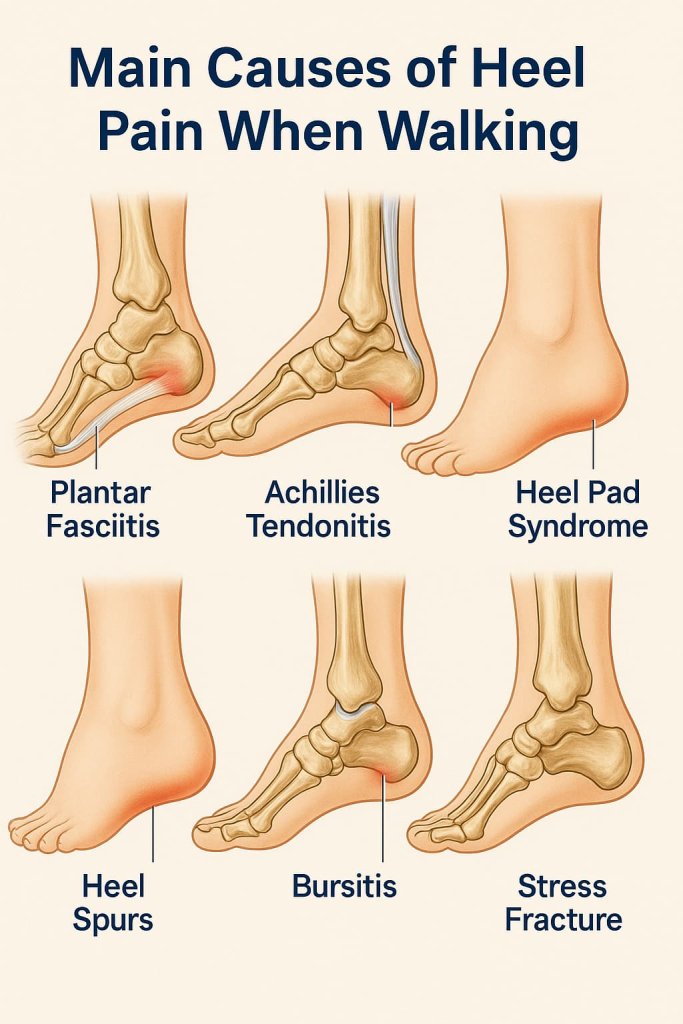
1. Plantar Fasciitis — The Leading Cause
- Overview: This accounts for up to 80% of heel pain cases (Cleveland Clinic).
- Mechanism: Microtears or degeneration in the plantar fascia (a thick band of connective tissue supporting the arch).
- Risk Factors:
- Sudden increase in walking/running distance
- Standing for long hours
- Flat feet or high arches
- Wearing worn-out shoes
- Typical Signs:
- Sharp “first-step” pain in the morning
- Pain that reduces after a few minutes of walking but returns after rest
- Example: An office worker who recently started a 10,000-step challenge develops morning heel pain—classic plantar fasciitis.
2. Achilles Tendonitis
- Overview: Irritation or inflammation of the tendon at the back of the ankle connecting the calf muscles to the heel bone.
- Triggers:
- Overtraining in sports like basketball or running
- Wearing high heels regularly, then switching to flat shoes
- Symptoms:
- Back-of-heel pain, swelling, and stiffness (especially in the morning)
- Pain that worsens with uphill walking or stair climbing
- Example: A weekend runner who suddenly adds hill sprints to training develops soreness above the heel.
3. Heel Pad Syndrome
- Overview: Loss of cushioning due to aging, overuse, or repeated impact.
- Symptoms:
- Deep, bruised feeling in the middle of the heel
- Worse when barefoot on hard floors
- Example: A warehouse worker who stands all day on concrete experiences dull heel pain.
4. Other Possible Causes
- Heel Spurs — Bone growths under the heel bone, sometimes linked to plantar fasciitis but not always painful.
- Bursitis — Inflammation of fluid-filled sacs around the heel from repetitive pressure.
- Stress Fractures — Tiny cracks in the heel bone, common in runners and military recruits.
- Nerve Entrapment — Tingling, burning, or numbness in the heel due to pinched nerves.
- Example: A hiker wearing too-tight boots develops burning heel pain from nerve compression.
- Source: Verywell Health – Heel Pain When Walking
Quick Relief at Home

1. RICE Protocol
- Rest: Avoid activities that trigger pain.
- Ice: Apply a cold pack for 15–20 minutes several times a day.
- Compression: Use an elastic bandage if swelling is present.
- Elevation: Raise your foot to reduce blood pooling and swelling.
2. Stretching & Mobility Drills
- Calf Wall Stretch: Stand facing a wall, one leg back, press heel into the ground for 30 seconds per side.
- Towel Stretch: Loop a towel around your toes, pull gently toward you while keeping knee straight.
- Rolling Massage: Use a frozen water bottle or tennis ball to massage the arch and heel. See exercise visuals in this Self.com guide.
3. Footwear & Insoles
- Replace worn-out shoes every 300–500 miles of use.
- Choose shoes with firm heel counters and shock-absorbing soles.
- Use orthotic insoles or silicone heel cups for extra cushioning.
4. Pain-Relief Support
- OTC NSAIDs (e.g., ibuprofen) may help reduce pain temporarily (only if appropriate for you).
- Foot massage improves blood flow and relaxes tight muscles.
When Home Remedies Aren’t Enough
If symptoms persist beyond 2–3 weeks or interfere with daily life, consult a healthcare professional.
Advanced Medical Options:
- Physical therapy to strengthen foot and ankle muscles
- Night splints to keep fascia stretched during sleep
- Shockwave therapy to stimulate healing
- Corticosteroid injections for severe inflammation
- PRP & Dextrose Prolotherapy — According to a 2025 KGMU study, both methods significantly reduced chronic plantar fasciitis pain, with PRP slightly outperforming dextrose, but costing 5–6x more (Times of India).
Prevention Strategies
- Increase training or walking volume by no more than 10% per week.
- Always warm up before exercise and stretch afterward.
- Maintain a healthy body weight to reduce stress on the heel.
- Use cushioned mats if standing for long hours at work.
- Rotate between at least two pairs of supportive shoes to avoid uneven wear.
FAQs
1. Can plantar fasciitis heal on its own?
Yes—most cases improve in 6–12 weeks with proper rest, stretching, and footwear changes.
2. Does walking make heel pain worse?
It depends on the cause. Gentle walking in supportive shoes may help circulation, but avoid long or high-impact walks until pain resolves.
3. Can I run with heel pain?
Not recommended. Running with heel pain can worsen the injury.
4. Is surgery ever needed?
Rarely—only if conservative treatments fail after 6–12 months.
5. Can losing weight help heel pain?
Yes—less body weight means less stress on the heel structures.
6. Are flat shoes harmful?
Yes, especially if worn long-term without cushioning or arch support.
7. How do I know if it’s a stress fracture?
Persistent pain that worsens with activity and eases with rest, often accompanied by pinpoint tenderness.
Conclusion
Heel pain when walking is not just a minor annoyance—it’s your body’s warning sign. Most cases can be resolved with home care, proper footwear, and early intervention. By identifying the root cause and making small daily adjustments, you can return to pain-free walking and protect your long-term foot health.
