Ankle pain when walking is most often caused by injuries, overuse, arthritis, nerve compression, or foot alignment issues — and most cases can be improved with proper care, targeted exercises, and preventive measures.
Your ankle is a highly complex joint made of bones, ligaments, tendons, and muscles that work together to provide stability and movement. It bears 1.5–3× your body weight with every step. This means even small issues can quickly turn into big problems if ignored. Understanding the cause — and acting early — can help you avoid chronic pain and long‑term damage.

This guide blends expert medical advice from trusted sources such as Cleveland Clinic, Hinge Health, Mayo Clinic, and the NHS with practical, real‑life tips.
How Common Is Ankle Pain When Walking?
Ankle pain is not limited to athletes. Office workers, teachers, retail employees, and seniors often experience it due to overuse, poor footwear, or joint wear and tear.
- Sports injuries: Up to ~20% of sports injuries involve the ankle (AOFAS).
- Re‑injury risk: After a first sprain, the ankle is more prone to future injury if rehab is incomplete.
- Long‑term impact: Repeated strain may contribute to arthritis and reduced mobility later in life.
Top Causes of Ankle Pain When Walking
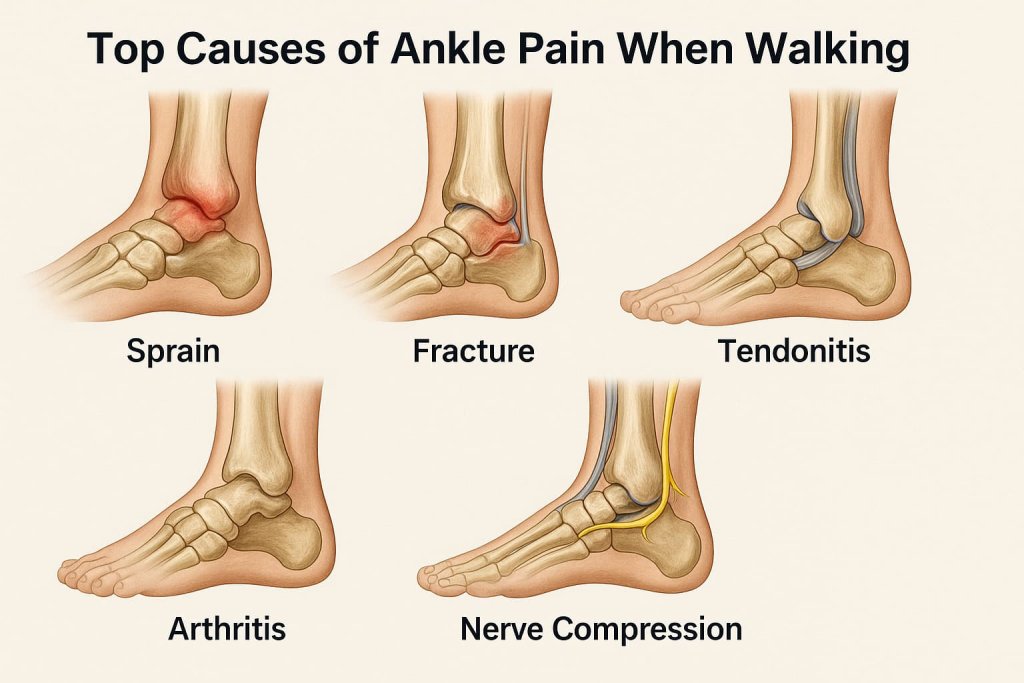
1) Sprains and Strains
Mechanism: A sprain stretches/tears ligaments; a strain injures muscles or tendons.
Real‑world example: Rolling your ankle stepping off a curb or on a trail.
Symptoms: Sudden pain, swelling, bruising, tenderness, instability when walking.
Why it matters: Poorly treated sprains weaken the ankle and raise re‑injury risk.
Quick tip: Follow the RICE protocol for the first 48 hours.
2) Fractures
Mechanism: A crack or break in one or more ankle bones (from stress fracture to complete break).
Example: Slipping on a wet surface and landing awkwardly.
Symptoms: Severe pain, swelling, bruising, inability to bear weight, possible deformity.
Action: Seek urgent care; fractures may require immobilization or surgery (Mayo Clinic).
3) Tendonitis (e.g., Achilles or Peroneal Tendonitis)
Mechanism: Repetitive strain causes tendon inflammation; sudden mileage or intensity jumps are common triggers.
Risk factors: Tight calves, flat feet, unsupportive shoes.
Symptoms: Gradual pain, morning stiffness, pain after walking or running.
Note: Untreated cases can progress to tendinosis (degeneration), which heals slower.
4) Arthritis
- Osteoarthritis: Wear‑and‑tear cartilage loss.
- Rheumatoid arthritis: Autoimmune inflammation.
- Post‑traumatic arthritis: Develops after injury.
Symptoms: Persistent ache, stiffness, swelling, reduced range of motion.
Management: Low‑impact exercise, weight management, and joint‑friendly routines (NHS).
5) Nerve Compression (Tarsal Tunnel Syndrome)
Mechanism: Tibial nerve compression in the tarsal tunnel.
Symptoms: Tingling, numbness, burning, shooting pain into the foot.
Triggers: Tight footwear, swelling after injury, flat feet.
Treatment: Orthotics, activity modification, physical therapy; surgery in resistant cases.
6) Overuse & Poor Foot Mechanics
Flat feet or high arches can alter weight distribution and strain the ankle. Long hours on hard floors and worn‑out shoes compound the problem.
Quick Relief Tips for Ankle Pain
1) RICE Protocol (First 48 Hours)
- Rest: Pause painful activities.
- Ice: 15–20 minutes every 2–3 hours for the first 48 hours.
- Compression: Elastic wrap or soft brace (ensure circulation).
- Elevation: Above heart level to reduce swelling.
2) Supportive Footwear
Choose shoes with firm heel counters, arch support, and cushioned midsoles. Replace them every 300–500 miles or when soles wear unevenly.
3) Orthotics & Braces
Quality over‑the‑counter insoles or custom orthotics help realign the foot and reduce ankle stress (APMA). Light ankle braces can add stability during recovery or sport.
4) Gentle Mobility & Strength Exercises
- Ankle circles & “alphabet” for range of motion.
- Calf raises (progress from two‑leg to single‑leg).
- Single‑leg balance (eyes open → eyes closed) to train stabilizers.
Progress gradually; avoid sharp pain (Hinge Health).
5) Anti‑Inflammatory Care
Favor omega‑3 rich foods (salmon, walnuts, chia), berries, and leafy greens. Topical anti‑inflammatory gels can help when used as directed by a clinician.
Prevention Strategies

Warm up & mobilize ankles before walking or exercise with light cardio and ankle circles.
Increase activity gradually — no more than 10% per week to avoid strain.
Avoid uneven terrain during recovery to reduce risk of twisting the ankle.
Maintain a healthy weight to lessen joint stress.
Strengthen hips and knees to support proper ankle alignment and stability.
When to See a Doctor
- Severe or sudden pain after injury.
- Inability to bear weight or a visible deformity.
- Worsening numbness/tingling or signs of infection.
- No improvement after 1–2 weeks of guided self‑care.
FAQs
1) Why do my ankles hurt only during walking?
Weight‑bearing reveals stress on injured or inflamed structures (ligaments, tendons, cartilage) that may not hurt at rest.
2) Is it safe to walk on a mild sprain?
Light walking may be tolerable, but pushing through pain can delay healing. Use support and follow RICE early on.
3) Can bad shoes cause ankle pain?
Yes. Worn soles and poor arch support change gait mechanics and increase joint strain. Replace shoes regularly.
4) Should I use ice or heat?
Ice for the first 48 hours after an acute flare; heat later for stiffness and muscle relaxation.
5) How long does recovery take?
Mild sprains: ~2–4 weeks; more severe injuries or chronic conditions can take months and may need professional care.
6) Are ankle braces helpful?
Yes — especially during sport or early return to activity after an injury.
7) Can stretching prevent ankle pain?
Routine calf/ankle mobility work improves flexibility and reduces strain, lowering injury risk.
Conclusion
Ankle pain when walking is manageable for most people with prompt care, supportive footwear, progressive strengthening, and smart training habits. Act early to prevent chronic issues. If pain persists or worsens, book a professional assessment for a tailored plan.
